La mortalità per malattie cardiovascolari (CVD) è la principale causa di morte in tutto il mondo, nei paesi ad alto, medio e basso reddito. Emerson Baptista e Bernardo Queiroz indagano in che misura i tassi di mortalità per malattie cardiovascolari nella popolazione adulta di un paese sono associati alle caratteristiche dei paesi circostanti.
Non-communicable diseases (NCDs) loom large in the global health landscape, posing formidable challenges to public health in both developed and developing nations (Lozano et al. 2012). Among these, cardiovascular diseases (CVDs) are the leading cause of mortality worldwide, exerting a significant impact on human lives and healthcare systems. In 2017, for instance, approximately 73% of global deaths, totaling 41 million, were attributed to NCDs, with CVDs accounting for a staggering 17.8 million deaths, representing 31.8% of overall global mortality (GBD 2018).
CVD: A global but unequally distributed problem
The prevalence of CVD-related mortality is not evenly distributed across the globe, with over three-quarters of CVD deaths occurring in low- and middle-income countries (WHO 2020). Despite ongoing efforts to mitigate the risk factors associated with CVDs, such as tobacco use, sedentary lifestyles, and poor diet, these conditions continue to affect populations, particularly in regions with socioeconomic disparities and limited access to healthcare.
Understanding the complex interplay of factors contributing to CVD mortality requires a nuanced examination of demographic, socioeconomic, behavioral, environmental, and physiological determinants. Several risk factors have been identified, including, among others, population aging, income inequality, urbanization, high blood pressure, high blood cholesterol levels, and tobacco use (Okwuosa et al. 2016; Roth et al. 2020; WHO 2020). While much of the existing research on CVD mortality has focused on developed countries, there is a growing recognition of the importance of understanding global trends and impacts also in low- and middle-income countries. These regions often face unique challenges, including limited healthcare infrastructure, inadequate access to preventive measures, and disparities in education and income levels, all of which contribute to the burden of CVDs.
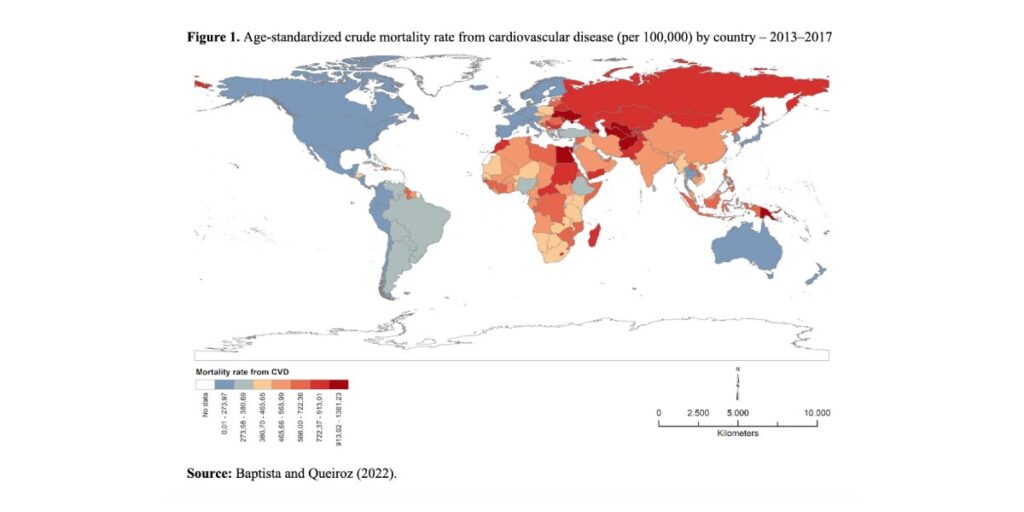
In a recent study (Baptista and Queiroz 2022), we assessed and juxtaposed several prevalent models utilized in mortality and health research, with the objective of determining whether national CVD mortality rates among the adult population (aged 30 years and above) correlate with the attributes of neighboring countries from 2013 to 2017. Their results highlighted persistent disparities in the crude mortality rate from cardiovascular disease (CMRCVD) across continents (Figure 1).
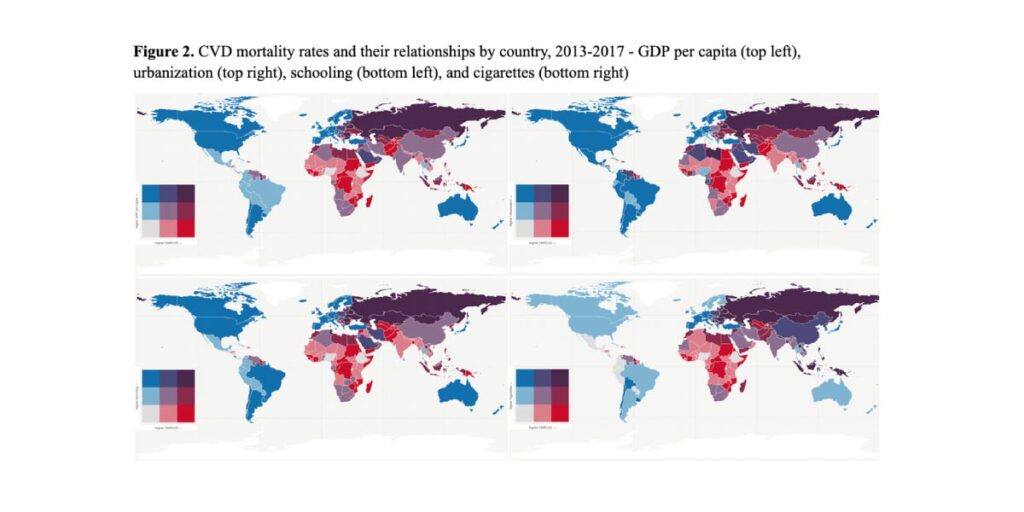
We also investigated the relationship between CVD mortality rates and GDP per capita (Figure 2, top left), urbanization (top right), schooling (bottom left), and cigarette use (bottom right) through bivariate maps. In the Americas, 66% of the countries are in the lowest quantile of CVD mortality rates and only two (Guyana and Haiti) are in the highest. Here, countries farther away from the equator tend to perform better, and so do most of the countries in Oceania except for Papua New Guinea which exhibits high CVD mortality rates along with low GDP per capita and urbanization levels, and where tobacco use is emerging as a significant risk factor. In Asia, there is heterogeneity in CVD mortality rates, reflecting the continent’s diverse socioeconomic, cultural, and demographic landscape. CVD mortality rates are higher in European countries, particularly those of Eastern Europe, and also in Africa, where, however, regional variation is particularly strong. Although Africa is still lagging in the epidemiological transition, the prevalence of chronic non-communicable diseases (NCDs), such as cardiovascular diseases, has increased in recent years, while the occurrence of communicable diseases has decreased.
Tackling the issue
Our findings underscore the importance of a coordinated global response to address the growing burden of CVDs. Policymakers, healthcare practitioners, and researchers must collaborate to implement evidence-based strategies that prioritize their prevention, early detection, and treatment. Moreover, efforts to strengthen health systems, improve data collection and surveillance, and address the social determinants of health are paramount for achieving sustainable progress in reducing CVD mortality rates worldwide. Aggregated country-level data may obscure regional variations within countries, highlighting the need for more granular analyses. Additionally, data quality and availability pose challenges, particularly in regions with limited healthcare infrastructure and inadequate vital statistics systems.
Efforts to address CVD mortality require a multifaceted approach that considers the broader social, economic, and environmental determinants of health. Investments in healthcare infrastructure and education, poverty alleviation, and public health initiatives are essential for reducing the burden of CVDs globally. Furthermore, targeted interventions aimed at mitigating known risk factors, such as tobacco control policies, promotion of healthy lifestyles, and access to affordable healthcare, are critical for stemming the tide of CVD-related mortality.
References
Baptista, E.A. & Queiroz, B.L. (2022). Spatial analysis of cardiovascular mortality and associated factors around the world. BMC Public Health 22, 1556 (2022). DOI: 10.1186/s12889-022-13955-7
GBD (Global Burden of Disease Collaborative Network). Global Burden of Disease Study 2017 (GBD 2017) Cause-Specific Mortality 1980–2017. Seattle: Institute for Health Metrics and Evaluation (IHME); 2018.
Lopez, A.D. & Adair, T. (2019). Is the long-term decline in cardiovascular-disease mortality in high-income countries over? Evidence from national vital statistics. Int J Epidemiol. 2019;48(6):1815–1823
Lozano, R. et al. (2012). Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;2012(380):2095–128.
Okwuosa, I.S. et al. (2016). Worldwide disparities in cardiovascular disease: challenges and solutions. Int J Cardiol. 2016;202:433–40.
Roth, G.A. et al. (2020). Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76(25):2982–3021.
WHO (World Health Organization). Cardiovascular diseases (CVDs). 2020.

